Diagnostic Imaging: How to image the oesophagus in practice settings
“Oesophageal transport is best-evaluated fluoroscopically” (C.S. Farrow)
Every radiologist would agree with this statement, but what if you have no access to fluoroscopy? Don’t panic! We can still obtain a lot of useful information with a common x-ray machine.
The normal oesophagus is difficult to see radiographically. Sometimes focal gas accumulation can be seen; this is often due to air swallowing in apprehensive animals. Fluid can occasionally collect in the caudal aspect of the normal oesophagus when dogs are in left recumbency. This fluid creates an elongated area of soft tissue opacity in the caudal aspect of the thorax that should not be confused with a mass or lung disease. This does not usually happen with the patient in right recumbency.
Generalised oesophageal distension can be induced by general anaesthesia, sedation or drugs affecting gastrointestinal motility. Therefore it is usually better to perform an oesophagram in conscious patients. If the patient is uncooperative or fractious care must be taken to avoid aspiration (giving contrast through a muzzle should be avoided).
Indications
Oesophageal contrast studies (“barium swallow”, oesophagraphy, oesophagography) can be performed to outline oesophageal lesions and conditions in the immediate vicinity of the oesophagus and to study swallowing difficulties and dysfunction.
Contrast media
Many contrast media are available and their use has been widely published.
Barium sulphate paste is supposed to give better results but sometimes it does not adhere to the mucosa as expected; it may also be difficult to find. Aspiration of paste can lead to asphyxiation and should not be used when aspiration is a concern.
Liquid barium sulphate suspension does not adhere well to the mucosa, but it is widely available in various concentrations (30% to 100% weight) and is relatively safe to use. An 85% weight suspension mixes well with fluid and flows around an obstruction.
Either liquid or paste can be mixed with food (preferably a similar food to the one the patient usually eats) and given as small boluses; this is useful when evaluating patients with problems in swallowing solids but not liquids.
Oral aqueous iodine solutions formulated for oral administration are relatively nontoxic in body cavities and can therefore be used when an oesophageal perforation is suspected. They are hypertonic and will induce pulmonary oedema when aspirated.
Nonionic organic iodinated media are isosmolar and relatively safe in case of aspiration, but they are more expensive and have a bitter taste (they are not formulated as oral agents) and can be difficult to administer.
Personal tip: as barium suspension is formulated for human use, it is usually flavoured with strawberry or vanilla neither of which is very palatable for our patients. Adding some anchovy paste can make it more palatable for dogs and cats.
Technique
Always take survey radiographs immediately before the contrast study is performed (this helps to check the exposure settings and allows assessment of the oesophagus and other thoracic structures). In addition to a lateral view, an oblique one, such as ventroleft-dorsoright or ventroright-dorsoleft, allows visualisation of the oesophagus without superimposition of the spine and sternum.
There are discordant opinions about sedation. Ideally a barium swallow should be performed without any drugs, but in the case of fractious patients what is the best approach? The truth is there not a “best answer”. Different radiologists have different views ranging from not performing the study at all, as any drug will affect oesophageal motility, to administering a small dose of tranquilizer and taking this into account when reviewing the study. (Difficult one as how are you supposed to know if what you see is the effect of the drug or not? Personally I only do it in conscious patients and avoid struggling with them; if they are fractious I stop and either try later or give up).
According to the size of the patient a bolus of 5-20 mls is given, inducing several complete swallows (allowing the patient to swallow each small bolus). If this is done with the patient on the radiology table my tip is to cover the table with an incontinence pad to avoid spillage of radiopaque contrast medium on the table; alternatively the swallow can be done with the patient on the floor and immediately after the last swallow it can be moved. If this procedure shows a normal oesophagus, the study can be repeated with small boluses of barium-coated food (prepare a few “meatballs” of soft dog food mixed with barium suspension and give 2-3 of them to the patient, allowing time to swallow each mouthful). Repeat radiographs as before.
A small amount of contrast can be seen in the lumen of a normal oesophagus. The canine mucosa appears as a series of longitudinal folds, while the feline one has a “herringbone” pattern in the caudal third.

Abnormal findings
Oropharyngeal dysphagia is characterised by accumulation of contrast medium in the oral cavity, oropharynx, pharynx or cranial oesophageal sphincter.
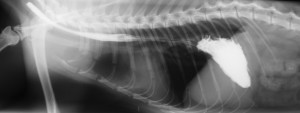
Megaoesophagus can be segmental or generalised. Segmental megaoesophagus can be caused by foreign bodies, oesophageal or perioesophageal masses, acquired strictures, segmental motor disease and congenital causes (vascular ring anomalies). In all these cases localised accumulation of contrast medium in a dilated portion of the organ is usually visible.
Generalised megaoseophagus can be congenital (hereditary in miniature Schnauzer and Fox Terrier) or acquired. The differential list for acquired megaoesophagus is quite extensive and includes: idiopathic, trauma, tetanus, myasthenia gravis, toxicosis (lead), immune mediated diseases, hypothyroidism, hypoadrenocorticism, thymoma, feline dysautonomia, dermatomyositis, gastrointestinal diseases (GDV, pyloric obstruction, hiatal hernia, oesophagitis), central neurological diseases (meningitis, trauma, neoplasia). Generalised megaoesophagus can be visible in survey radiographs as two thin parallel lines running caudally beyond the diaphragm. When the lumen is full of gas it may be more difficult to see than when fluid or radiopaque food material accumulates in the lumen. Megaoesophagus is usually easy to detect with radiopaque contrast medium.


When perforation of the oesophageal wall is present, contrast medium is visible outside of the lumen.
With hiatal hernia a soft tissue mass is often present in the dorsocaudal aspect of the thoracic cavity. These hernias are often dynamic and may appear different (or not appear at all) in subsequent radiographs. Barium will allow identification of the misplaced gastric fundus; the caudal oesophageal sphincter is recognised as a focal narrowing of the barium column. Gastric rugal folds can also be seen.